Canan Dagdeviren on Miniaturized Neural Drug delivery System (MiNDS)
It is now common knowledge that neurological disorders arise from the dysregulation of neural circuits, rather than from a single afflicted region of the brain. Conventionally, drugs for these diseases are administered orally or intravenously, with drug treatments distributed throughout the body. Such approaches to drug delivery lack the spatial resolution to target specific dysfunctional neural pathways, resulting in delivery kinetics that are too coarse to adequately compete with the rapidly changing activity in the brain.
Currently, clinical methods of drug delivery result in: (1) systemic toxicity; (2) rapidly escalating dosing regimens; and (3) limited therapeutic efficacy. Despite some improvements in our understanding of the pathophysiological effects associated with neurodegenerative disorders, there is a deficit of suitable technology that can integrate with the rapid dynamics of neural circuits.
In this research published at Science Translational Medicine, we aimed to bridge the gap between cutting-edge neuroscience research and novel engineered devices by developing a multi-functional neural system capable of exploring—and eventually treating—Parkinson’s disease. This multi-functionality makes it a powerful tool to modulate specific neural pathways in animal models.
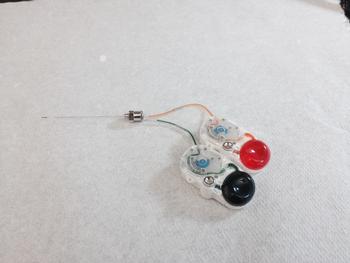
The biocompatible, remotely controllable Miniaturized Neural Drug delivery System, called MiNDS, permits dynamic neural adjustment with pinpoint spatial resolution and cell-type specificity. With dual chemical-delivery channels and an electrode embedded in a stainless-steel needle carrier, microfabricated MiNDS can chemically modulate local neuronal activity and related behavioral changes in animal subjects while simultaneously recording neural activity to enable feedback control. In this way, it becomes possible to decrease both systemic toxicity and therapy time.
MiNDS is customizable, with high-bending stiffness, high aspect ratio, and an adjustable number of channels, which allows it to reliably reach deep brain structures in small- and large-animal models without the need of an extraneous guide tube to implant. Our collective infusion findings via three-dimensional positron emission tomography imaging show the capability of MiNDS to maintain a localized delivery. Moreover, MiNDS avoids the problems of backflow encountered in acute infusions and can deliver nano-liter quantities of drugs in a tunable, repeatable manner.
In my research group, Conformable Decoders, at the MIT Media Lab, my students and I are also working on integrating small, conformable sensors at the tip of MiNDS to monitor real-time phenotypic parameters such as temperature, pressure, stiffness during drug infusions, and an integrated tissue retrieval channel for obtaining brain biopsies. Such multimodal capabilities would allow for more in-depth investigation into the pathology of neurological conditions in vivo as well as a novel drug exploration system for pharmaceutical research and development.
The customizable feature of our MiNDS could open new routes to deliver not only light but also chemicals and electricity to other organs (not limited only to the brain) with pinpoint spatiotemporal resolution.
So far, we conducted pre-clinical trials in small (rodent) and large (nonhuman primate) animal models. Long-term (beyond 2 months) studies in small and large animal models are the next steps, and then the clinical studies after having permissions to do so. I would assume that we need 5 to 10 years to have this technology to be used in clinics by the doctors.